What is diabetes?
“Diabetes is a condition that occurs when your body does not produce enough insulin or your body is not able to use the insulin produced effectively, resulting in blood glucose (blood sugar) levels being too high”. Blood glucose levels are measured in mg/dL or mmol/L.
There are two most common types of Diabetes:
- Type 1 Diabetes: Your body produces little to no insulin. Insulin must be taken each day to keep blood glucose levels in the normal range.
- Type 2 Diabetes: Your body makes insulin but it may not work properly or be enough to keep blood glucose levels in the normal range.
What is Insulin?
Insulin is a hormone made by your body. Without insulin or enough insulin, your body is not able to use sugar (glucose) from the food that you eat to create energy, or to store glucose for future use.
Why is Insulin Important?
Insulin helps keep your blood glucose level from getting too high(hyperglycemia). Prolonged hyperglycemia can cause the complications we want to avoid. People with type 1 diabetes need to take insulin everyday in order to remain healthy. People with type 2 diabetes may also need to take insulin to control blood glucose levels.
Types of Insulin
There are four main types of insulin. Each type acts differently in the body:
- rapid-acting
- short-acting
- intermediate-acting
- long-acting
Each type has a different:
- Onset: how quickly it starts working after injection
- Peak: when it works most effectively, and
- Duration: how long it works in your body
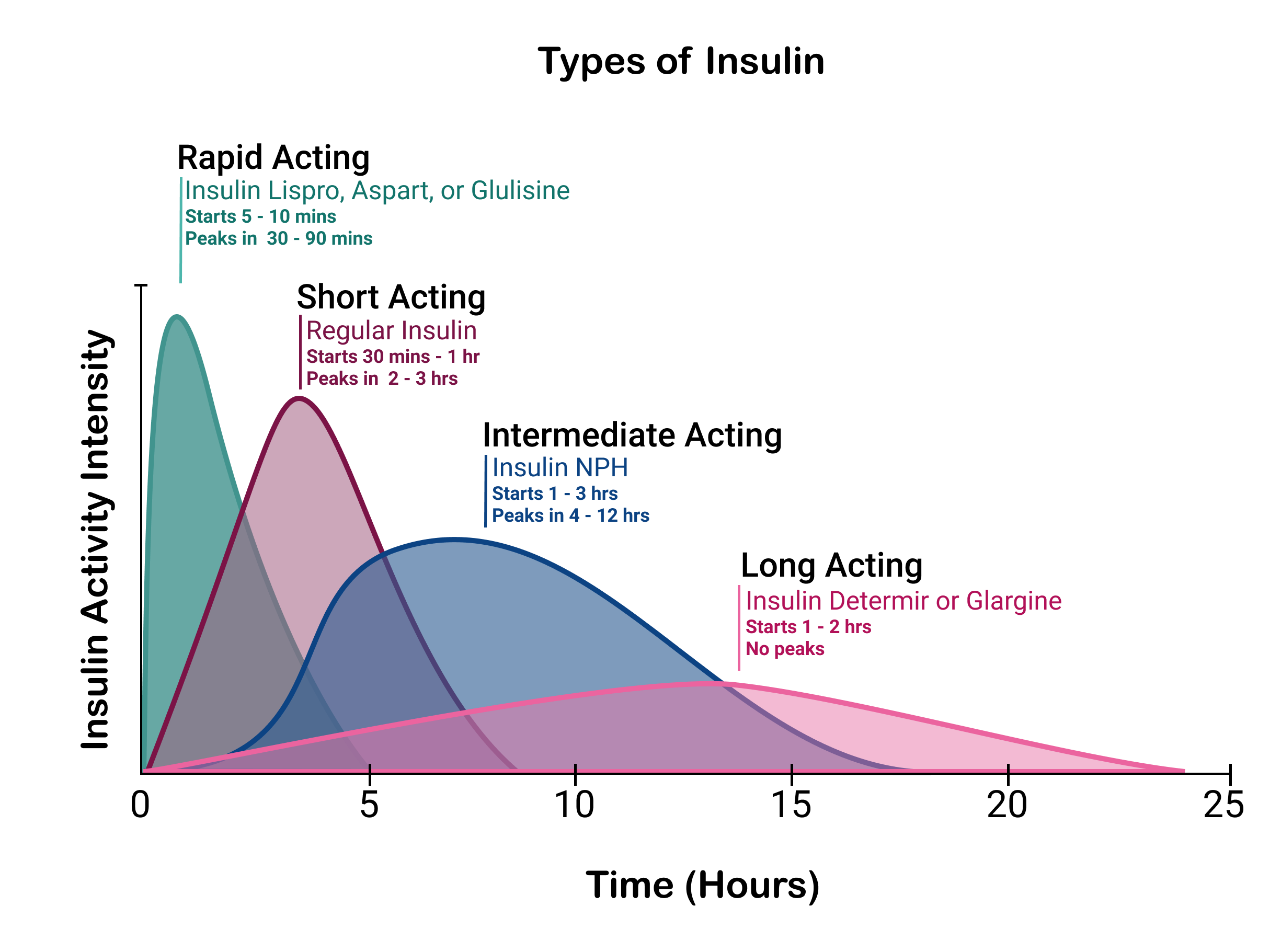
Bolus insulin (rapid- and short-acting insulin): These insulins work quickly and have a shorter duration compared to other insulins. These insulins are used to control blood glucose levels at meal time.
Basal insulin (intermediate-acting and long-acting): These insulins work more slowly and last longer; they provide “background” action to help keep blood glucose levels from going too high throughout the day and at night.
Note: Basal insulin is usually taken as a shot. However if you are on a pump, your basal insulin would be rapid-acting insulin given in small amounts throughout the day.
Our goal is to show how insulin dosing and timing for meals is important.
We will focus on rapid-acting insulin which is usually taken at meal times.
Insulin Activity Curve
The insulin activity curve shows when the insulin is working over time. It's important for understanding when to take insulin to best manage your blood glucose levels at meal time.
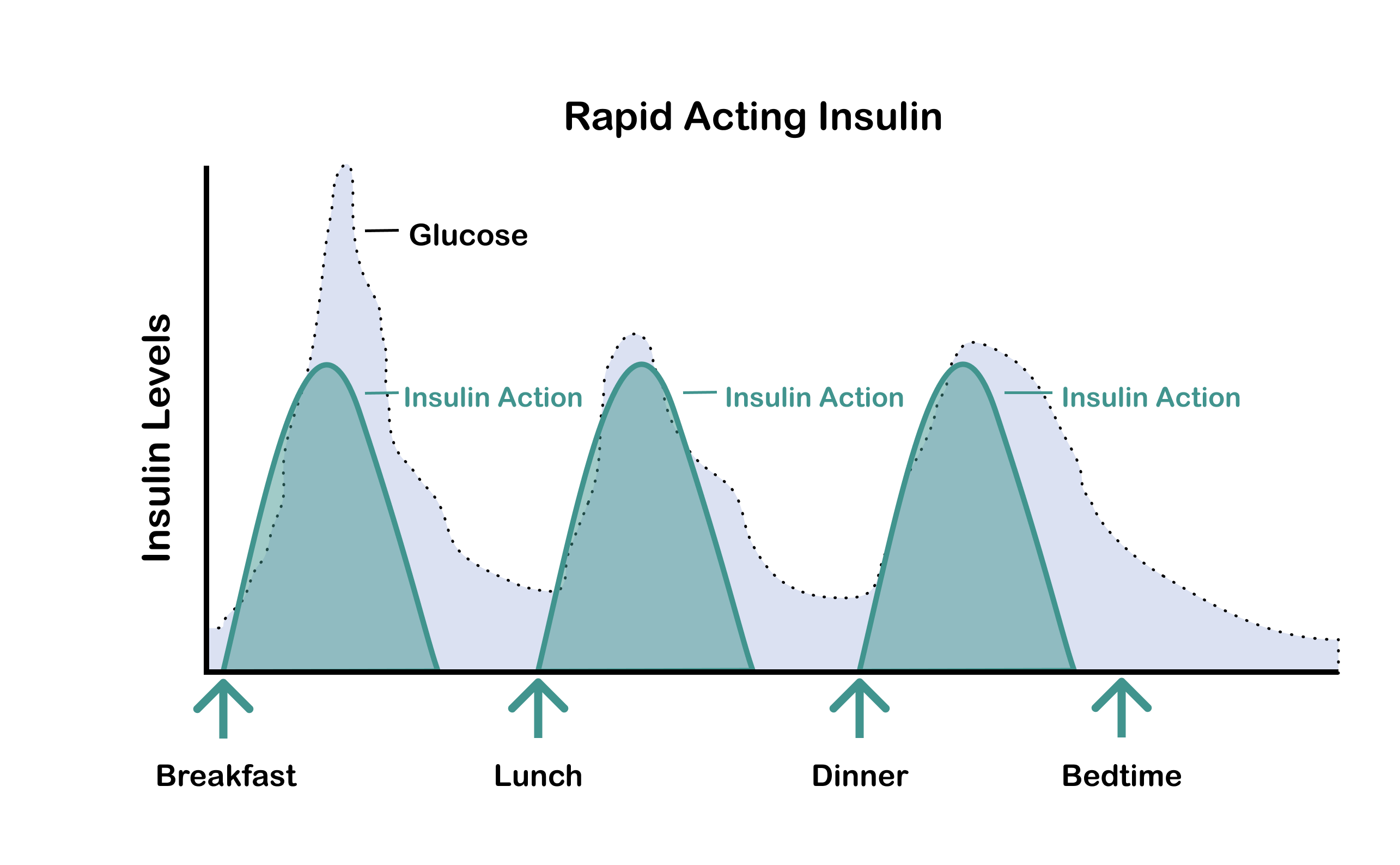
Rapid-acting insulin typically begins working about 5 - 20 minutes after it is taken, peaks within about 30 - 90 minutes, and is active in the bloodstream for about 3.5-5 hours.
Because rapid-acting insulin works more quickly, peaks higher and action time is shorter, it prevents blood glucose from going high at meal time.
Disclaimer: Rapid-acting insulin works differently for everyone, so your activity curve may vary. Please refer to your healthcare provider for more information.
Bolus Timing
A bolus is the dose of insulin you take when you eat to keep blood sugar levels controlled at meal time. Your bolus needs to act quickly to balance out the carbohydrates raising your blood sugar, so rapid-acting or short-acting insulin is typically used.
Pre-bolusing is the term used to describe taking your rapid-acting insulin dose before you eat, usually 15-20 minutes before depending on the circumstances. Pre-bolusing gives your insulin time to be absorbed in your body so that when you start eating, it’s ready to lower your blood glucose level.
Your health care provider will help you figure out when you should bolus. In some situations, taking insulin during or following a meal may be recommended. Talk to your doctor about what works best for you.
Disclaimer: There are many other factors that also affect glucose levels, such as exercising, type of food, illness, stress and medication. However, the focus for this tool is insulin.
See how different bolus time affects your blood glucose

Bolus Dosing
Different foods will affect your blood glucose levels differently, so your bolus dose needs be matched to what you're eating. Learning how to count carbohydrates (which raise your blood glucose) can help you figure out how much insulin to take to keep your blood glucose in range at meal time.
For this tool, we use a typical American meal as a standard meal (about 45-75 grams of carbohydrates). Different people will require different amounts of carbohydrates and insulin.
Disclaimer: The numbers used in this tool are for education purposes only. Please ask your healthcare provider for more information.
See how different bolus dose affects your blood glucose
Time In Range
Time-in-Range is the percentage of time your blood sugar levels are within a target range. Our tool features a target range of 70 to 180 mg/dL, the recommended time-in-range by American Diabetes Association (ADA).
The goal is for people with a continuous glucose monitor (CGM) to increase time spent in-range, while reducing the time spent below or above target range The ADA recommendation is to spend at least 70% of the day in the target range of 70 to 180 mg/dL. Time-in-range is a useful way to track your progress and to provide insights into what behaviors and choices affect your glucose values. Time-in-range goals vary; talk to your healthcare provider.
Disclaimer: Your blood sugar targets may be different depending on your age, any additional health problems you have, and other factors. Be sure to talk to your health care team about which targets are best for you.